Experiencing constipation one day and diarrhea the next can feel confusing and concerning. You might wonder if these opposing symptoms mean something is seriously wrong, or why your digestive system seems unable to find a normal rhythm.

The alternating pattern of constipation and diarrhea most commonly indicates irritable bowel syndrome with mixed bowel habits (IBS-M), though it can also result from paradoxical diarrhea where liquid stool leaks around hardened, impacted stool. Both conditions share a similar underlying issue: your digestive system struggles to maintain consistent motility and function. In IBS-M, your intestinal contractions alternate between being too slow and too fast. With paradoxical diarrhea, severe constipation creates a blockage that allows only liquid waste to pass around it, mimicking true diarrhea when the core problem is actually constipation.
Understanding the specific mechanism behind your symptoms matters because it determines which treatments will actually help. This article examines the physiological reasons these symptoms alternate, identifies warning signs that require medical attention, and explains evidence-based approaches that address the root causes rather than just treating each symptom as it appears.
Medical Disclaimer: This article provides general information and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider regarding your specific symptoms and health concerns.
Understanding Why Constipation Alternates with Diarrhea
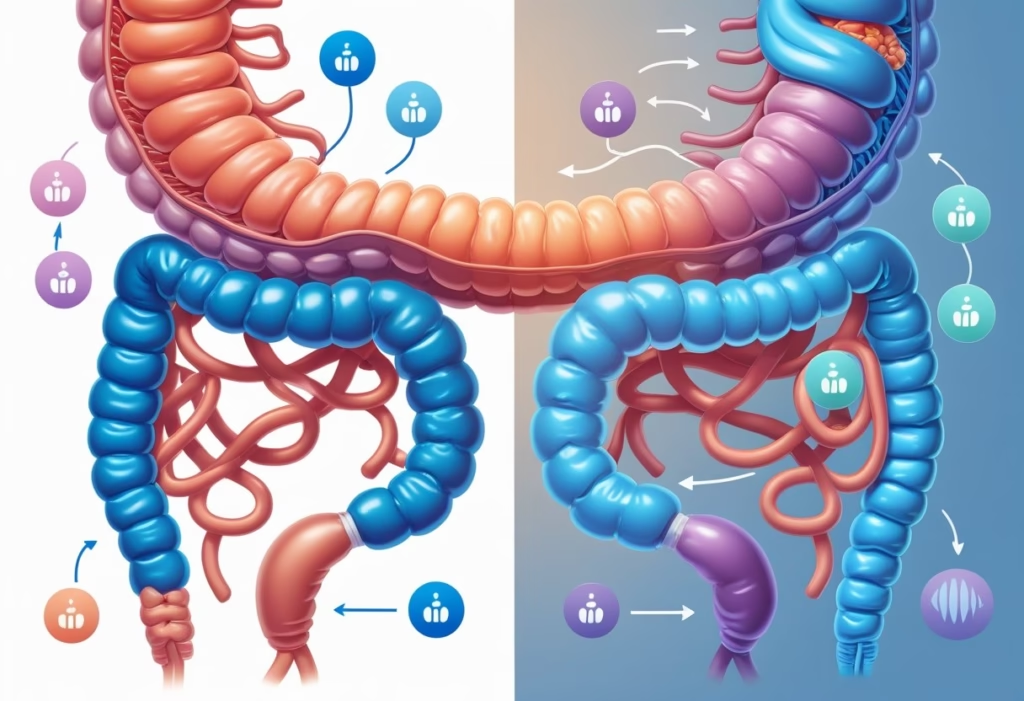
The alternation between constipation and diarrhea occurs through two primary mechanisms: disrupted intestinal motility that creates mixed bowel habits, and a physical blockage scenario where liquid stool bypasses hard, impacted stool.
How Mixed Bowel Habits Develop
Your intestines rely on coordinated muscle contractions to move waste through your digestive system at a consistent pace. When this coordination becomes disrupted, you experience what doctors call mixed bowel habits.
The intestinal wall contains nerve cells and muscle layers that communicate with your brain through the gut-brain axis. Stress, dietary changes, or sensitivity issues can alter these signals, causing your intestines to contract either too quickly or too slowly at different times.
When contractions speed up, your intestines don’t absorb enough water from waste, producing watery stool. When they slow down, too much water gets absorbed, creating hard stools that are difficult to pass. This pattern commonly occurs in IBS-M (irritable bowel syndrome with mixed bowel habits), where you experience both extremes within the same week or even the same day.
Your diet plays a direct role in worsening this pattern. Eating large amounts of fermentable carbohydrates can trigger rapid transit and diarrhea, while suddenly reducing fiber intake often leads to constipation. The cycle perpetuates itself because dietary choices that help one symptom may worsen the other.
Paradoxical Diarrhea and Overflow Mechanism
Overflow diarrhea, also called paradoxical diarrhea, happens when severe constipation creates a blockage in your rectum or lower colon. Hard, impacted stool forms a physical barrier that prevents normal bowel movements.
Your body continues producing digestive waste and mucus above this blockage. The liquid portion of newer stool cannot pass the hardened mass, so it seeps around the edges and leaks out as watery diarrhea. You might think you have diarrhea when you actually have significant constipation.
This condition affects approximately 2% of people with chronic constipation. You may notice you’re passing small amounts of liquid stool frequently while feeling bloated or having incomplete evacuation. Many people mistakenly take anti-diarrheal medication, which makes the underlying constipation worse.
Warning signs of fecal impaction include: abdominal pain, inability to pass stool despite feeling the urge, leaking liquid stool, and rectal pressure. If you suspect overflow diarrhea, see a doctor promptly rather than treating the liquid stool alone, as the impaction requires proper medical removal.
This information is for educational purposes and does not replace professional medical advice. Consult a healthcare provider for diagnosis and treatment of digestive symptoms.
Common Causes of Alternating Constipation and Diarrhea

Several medical conditions and factors can disrupt normal bowel patterns, causing them to swing between constipation and diarrhea. The most common culprits include functional bowel disorders, physical blockages, medications that alter gut motility, and daily habits that affect digestive health.
Irritable Bowel Syndrome and Subtypes
IBS represents the most frequent cause of alternating bowel habits, affecting approximately 16% of adults. This functional disorder disrupts the normal communication between your brain and gut, causing irregular intestinal contractions that change stool consistency and frequency.
IBS-M (mixed bowel habits) specifically describes the pattern where you experience both hard, lumpy stools and loose, watery stools within the same time period. This subtype differs from IBS-C (constipation-predominant) and IBS-D (diarrhea-predominant), which each favor one symptom pattern.
The alternating pattern happens because your intestinal muscles contract irregularly. When contractions slow down, stool stays in your colon longer, losing water and becoming hard. When contractions speed up excessively, stool moves through too quickly, preventing proper water absorption.
Symptoms typically improve after bowel movements and worsen with stress, hormonal changes, or trigger foods. You need to track your symptoms for at least three months before doctors can diagnose IBS using Rome IV criteria, which requires abdominal pain occurring at least once weekly alongside changes in stool frequency or appearance.
Fecal Impaction and Blockages
Fecal impaction creates a paradoxical situation where constipation actually causes diarrhea. Hard stool becomes lodged in your rectum or colon, forming a blockage that prevents normal bowel movements.
Liquid stool from higher in your digestive tract seeps around this impacted mass, leaking out as what appears to be diarrhea. This overflow diarrhea misleads many people into taking anti-diarrheal medications, which worsens the underlying blockage.
Common causes of impaction include:
- Chronic constipation left untreated for weeks
- Overuse of constipating medications
- Inadequate fluid intake combined with high fiber consumption
- Ignoring the urge to defecate repeatedly
- Limited mobility in elderly or bedridden individuals
The impacted stool must be removed before normal bowel function returns. Taking laxatives without addressing severe impaction can cause complications, so you should see a doctor if you haven’t had a complete bowel movement in over a week or experience rectal pain with leaking liquid stool.
Medication Effects on Bowel Patterns
Many medications disrupt your normal bowel rhythm by altering gut motility, fluid balance, or intestinal bacteria. Antibiotics represent a frequent cause because they eliminate beneficial gut bacteria alongside harmful ones, leading to temporary digestive chaos that manifests as alternating symptoms.
Medications that commonly cause constipation:
- Opioid pain relievers
- Antacids containing calcium or aluminum
- Antidepressants (especially tricyclics)
- Iron supplements
- Calcium channel blockers
Medications that commonly trigger diarrhea:
- Antibiotics (particularly broad-spectrum types)
- Metformin for diabetes
- Proton pump inhibitors for acid reflux
- NSAIDs taken regularly
When you start or stop these medications, your bowel patterns may fluctuate unpredictably. The timeline matters—if symptoms began within days of starting a new medication, that drug likely contributes to the problem. Stopping antibiotics after a course can trigger constipation as your gut bacteria population rebuilds.
Never stop prescribed medications without medical guidance, but do inform your doctor if bowel changes interfere with your daily life.
Dietary and Lifestyle Factors
Your diet directly influences stool consistency and transit time through multiple mechanisms. Food intolerances create inflammation that speeds up intestinal contractions, while inadequate fiber intake slows everything down.
Celiac disease and ulcerative colitis cause alternating patterns because inflammation flares and subsides. During active inflammation, you experience diarrhea. Between flares, slower motility or scarring can cause constipation.
Inconsistent fiber intake creates problems worse than eating too little fiber consistently. Suddenly adding whole grains without adequate hydration pulls water into your colon, initially causing loose stools, then leading to hard, bulky stools that move slowly.
Your fluid intake matters more than most people realize. Dehydration makes stool hard regardless of fiber consumption. When you then drink large amounts of water, the sudden fluid influx can trigger loose stools before your body regulates absorption.
| Factor | Effect on Constipation | Effect on Diarrhea |
|---|---|---|
| Inadequate hydration | Worsens significantly | Minimal direct effect |
| Sudden fiber increase | Initially may help | Can trigger temporarily |
| Irregular meal timing | Disrupts regularity | Can trigger episodes |
| Sedentary lifestyle | Major contributor | Minimal direct effect |
Regular physical activity stimulates intestinal contractions through multiple pathways, including increased blood flow and mechanical jostling of abdominal contents. When you’re inactive for days then suddenly active, your gut may respond with temporary diarrhea.
Stress and sleep disruption alter gut motility through your vagus nerve. Poor sleep consistently correlates with IBS symptom worsening because it disrupts the hormones that regulate digestion.
Medical Disclaimer: This information is for educational purposes and does not replace professional medical advice. Consult a healthcare provider for diagnosis and treatment of digestive symptoms, especially if you experience blood in stool, unintentional weight loss, or symptoms that awaken you from sleep.
Clinical Features and Warning Signs
Recognizing the pattern of alternating bowel habits requires attention to specific symptoms and their frequency. Most people experience mild digestive changes occasionally, but certain features indicate when medical evaluation becomes necessary.
Symptoms of Alternating Bowel Habits
You’ll typically notice a pattern where hard, difficult-to-pass stools alternate with loose, watery bowel movements over days or weeks. This cycle often includes abdominal pain that improves after you pass stool, which distinguishes it from other digestive conditions. The pain usually occurs in the lower abdomen and may shift in location.
Your stool consistency varies significantly during these episodes. You might pass lumpy, hard stools fewer than three times per week during constipated phases, then experience three or more loose stools daily during diarrhea phases. Some people develop symptoms of paradoxical diarrhea, where liquid stool leaks around impacted hard stool.
Abdominal discomfort frequently accompanies these bowel changes, presenting as cramping, bloating, or a sensation of incomplete evacuation. The discomfort intensity varies throughout the day and often worsens after meals. You may also experience increased gas production and audible bowel sounds during symptom flares.
When to Seek Medical Evaluation
Schedule an appointment with your doctor if you notice blood in stool, whether bright red or dark and tarry. This signals potential inflammation, hemorrhoids, or more serious conditions requiring immediate assessment. Unexplained weight loss of more than 5% of your body weight within six months warrants prompt evaluation, as this rarely occurs with simple functional bowel disorders.
Seek medical attention for symptoms starting after age 50, persistent fever, or signs of anemia such as fatigue, weakness, and pale skin. Fecal incontinence that affects your daily activities requires professional management. Nighttime symptoms that wake you from sleep differ from typical functional bowel patterns and need investigation.
A family history of inflammatory bowel disease or colorectal cancer increases your risk for conditions beyond simple IBS-M. Recent antibiotic use followed by persistent bowel changes may indicate infection requiring treatment. New or significantly different pain patterns from your usual symptoms should prompt reevaluation.
Associated Abdominal Discomfort
The abdominal pain linked with alternating bowel habits typically follows a recognizable pattern. You’ll notice cramping that builds before bowel movements and subsides afterward, unlike constant pain from other conditions. This relief after defecation happens because passing stool reduces intestinal distension.
Your discomfort often intensifies during periods of increased stress or anxiety, as the brain-gut connection directly affects intestinal sensitivity. Eating large meals or specific trigger foods like high-fat dishes, caffeine, or artificial sweeteners commonly worsens symptoms within 30 minutes to two hours.
The pain rarely occurs at night during sleep, which helps distinguish functional bowel disorders from structural problems. If you experience severe, unrelenting pain or pain that progressively worsens, this suggests conditions requiring different treatment approaches than standard alternating bowel habit management.
This information is for educational purposes and does not replace professional medical advice. Consult a healthcare provider for proper diagnosis and treatment of your symptoms.
Diagnostic Approaches and Tests
Healthcare professionals use specific criteria and testing methods to determine whether alternating bowel habits stem from IBS or another digestive condition. The diagnostic process typically starts with symptom evaluation using standardized criteria, then moves to laboratory tests and imaging when red flags appear.
Using Rome IV Criteria
The Rome IV criteria serve as the primary diagnostic framework for IBS when you experience alternating constipation and diarrhea. Your doctor will assess whether you’ve had abdominal pain or discomfort at least once per week during the past three months, with symptoms starting at least six months before diagnosis.
The criteria require at least two of these features: pain that improves after a bowel movement, changes in how often you pass stool, or changes in stool appearance. Based on your predominant symptoms, you’ll be classified into IBS-C (constipation), IBS-D (diarrhea), IBS-M (mixed), or IBS-U (unclassified).
Your doctor diagnoses IBS-M specifically when more than 25% of your bowel movements are hard or lumpy (constipation) and more than 25% are loose or watery (diarrhea). This classification matters because it determines which treatments will work best for your specific pattern.
A common mistake is assuming these criteria alone confirm IBS. Your doctor must first rule out alarm features like blood in stool, unintentional weight loss, or family history of colon cancer before making this diagnosis.
Laboratory and Stool Tests
Blood tests check for underlying conditions that mimic IBS symptoms. Your doctor will typically order thyroid function tests (TSH) because hypothyroidism commonly causes constipation, and calcium levels since high calcium can also slow bowel movements.
A complete blood count identifies anemia, which might indicate bleeding in your digestive tract rather than simple IBS. Inflammatory markers like C-reactive protein or fecal calprotectin help distinguish between IBS and inflammatory bowel disease.
Stool tests become necessary when you have additional warning signs. These include tests for infections (bacterial, viral, or parasitic), blood that’s not visible to the naked eye, and markers of inflammation. If you recently used antibiotics or traveled internationally, your doctor may specifically test for Clostridioides difficile or parasites.
Celiac disease testing through blood work makes sense if you have diarrhea-predominant symptoms, since celiac can cause similar bowel pattern changes. Many patients waste time on restrictive diets before getting this simple blood test.
Endoscopy: Colonoscopy and Sigmoidoscopy
Colonoscopy examines your entire colon using a flexible tube with a camera. Your doctor recommends this procedure if you’re over 50 with new symptoms, have blood in your stool, experience nighttime symptoms that wake you, or show signs of anemia.
This test helps rule out colon cancer, inflammatory bowel disease (ulcerative colitis or Crohn’s disease), and microscopic colitis—conditions that cause similar alternating bowel patterns but require different treatments. Biopsies taken during the procedure can detect inflammation not visible to the camera.
Sigmoidoscopy examines only the lower portion of your colon and rectum. It’s less invasive than a full colonoscopy but provides limited information. Your doctor might choose this option if your symptoms and physical exam suggest problems concentrated in the lower digestive tract.
Neither test is routinely needed for typical IBS symptoms without red flags. Requesting these procedures when you don’t have alarm features rarely changes the diagnosis or treatment plan, and the preparation process can temporarily worsen your symptoms.
Medical Disclaimer: This information is for educational purposes and should not replace professional medical advice. Consult your healthcare provider for diagnosis and treatment specific to your condition.
Treatment Strategies and Management
Managing alternating constipation and diarrhea requires addressing both extremes without worsening either condition. The key is stabilizing bowel function through targeted dietary changes, selecting medications that work for mixed patterns, and establishing consistent routines that support regularity.
Dietary Modifications and Fiber Intake
Fiber intake needs careful calibration when you experience both constipation and diarrhea. Soluble fiber typically works better than insoluble fiber because it normalizes stool consistency in both directions—it adds bulk to loose stools while softening hard ones.
Psyllium is often the most effective choice for mixed bowel patterns. Start with small doses (around 3-5 grams daily) and increase gradually to avoid bloating or gas. Take it with adequate water, as insufficient fluid can worsen constipation.
Foods rich in soluble fiber include:
- Oats and oat bran
- Ground flaxseed
- Bananas (ripe)
- Cooked carrots
- Sweet potatoes
A common mistake is adding too much insoluble fiber (like wheat bran or raw vegetables) too quickly, which can trigger diarrhea episodes. Another error is eliminating all fiber during diarrhea phases, which often prolongs the cycle rather than resolving it.
Avoid excessive caffeine, alcohol, and high-fat foods, as these can accelerate intestinal transit and worsen diarrhea. Dairy products may trigger symptoms if you have lactose intolerance, which frequently coexists with bowel pattern changes.
Medications for Mixed Bowel Patterns
Medication selection depends on which symptom predominates, though some options help stabilize both patterns. Bulk-forming laxatives like psyllium or methylcellulose often provide the safest starting point because they normalize stool consistency without causing rebound effects.
Osmotic laxatives (polyethylene glycol, lactulose) work for constipation-dominant phases by drawing water into the colon. They’re generally gentler than stimulant laxatives and don’t cause dependency. Use them during constipation episodes but reduce or stop during diarrhea phases.
Avoid stimulant laxatives (senna, bisacodyl) when possible, as they can trigger cramping and diarrhea, perpetuating the cycle. Stool softeners like docusate provide minimal benefit for most people and rarely address the underlying pattern.
For cramping and urgency, antispasmodics (dicyclomine, hyoscyamine) taken before meals can reduce intestinal spasms. Peppermint oil capsules (enteric-coated, 180-200 mg) work similarly with fewer side effects, though they may worsen heartburn.
Tricyclic antidepressants in low doses (10-25 mg amitriptyline or nortriptyline) can slow intestinal transit and reduce pain perception. These work best when diarrhea predominates or when anxiety worsens symptoms.
Lifestyle Adjustments and Bowel Routines
Establishing a consistent bowel routine helps regulate irregular patterns. Attempt a bowel movement at the same time daily, ideally 15-30 minutes after breakfast when the gastrocolic reflex is strongest. This trains your colon to respond predictably.
Physical activity stimulates peristalsis and reduces constipation risk. Aim for 20-30 minutes of moderate exercise most days—walking, swimming, or cycling all work. Sitting for prolonged periods slows intestinal movement and worsens constipation phases.
Stress directly affects bowel function through the gut-brain axis. High stress levels increase intestinal sensitivity and disrupt motility patterns. Techniques like diaphragmatic breathing, progressive muscle relaxation, or cognitive behavioral therapy can reduce symptom severity.
Never ignore the urge to defecate, as delaying bowel movements allows stool to harden and restarts the constipation-diarrhea cycle. Keep a symptom diary tracking food intake, stress levels, and bowel patterns to identify personal triggers.
See a doctor if you experience blood in stool, unintended weight loss, symptoms that awaken you from sleep, or if you’re over 50 with new-onset symptoms—these warrant evaluation for other conditions.
Medical Disclaimer: This information is for educational purposes and does not replace professional medical advice. Consult your healthcare provider before starting any treatment regimen.
Potential Complications and Special Considerations
Alternating bowel patterns can lead to serious health risks when left unmanaged, including fecal impaction, electrolyte imbalances, and damage to the intestinal wall. Certain medical conditions increase vulnerability to these complications.
Risks of Prolonged Constipation and Diarrhea
Fecal impaction develops when hardened stool becomes lodged in your colon or rectum. This occurs because chronic constipation allows stool to accumulate and dry out. The impaction can trigger paradoxical diarrhea, where liquid stool leaks around the blockage and exits your body.
Straining during constipation causes the Valsalva maneuver, which slows your heart rate and increases venous pressure. This can lead to hemorrhoids, anal fissures, and rectal bleeding. The constant straining damages blood vessels in the rectal area.
Chronic diarrhea depletes your body of essential electrolytes like sodium, potassium, and magnesium. These losses cause weakness, irregular heartbeat, and confusion. Dehydration compounds these effects because your intestines cannot absorb water properly during frequent loose stools.
Seek immediate medical attention if you experience blood in stool, fever above 101°F, severe abdominal pain, signs of dehydration (dark urine, dizziness), or inability to pass stool or gas for several days.
Complications in Specific Conditions
People with inflammatory bowel disease (IBD) face higher risks of bowel obstruction and toxic megacolon when constipation develops. The inflammation weakens intestinal walls, making them susceptible to perforation during severe constipation. Alternating symptoms in IBD patients often signal disease flares requiring medication adjustments.
Malabsorption disorders like celiac disease worsen during diarrhea episodes because your intestinal lining cannot absorb nutrients effectively. This creates vitamin deficiencies (particularly B12, iron, and fat-soluble vitamins) and unexplained weight loss.
Older adults experience complications more rapidly due to reduced intestinal motility and decreased thirst response. They develop dehydration and electrolyte imbalances faster than younger individuals, increasing fall risk and confusion.
This information is for educational purposes only and does not replace professional medical advice. Consult a healthcare provider for diagnosis and treatment of gastrointestinal symptoms.
